Prior to any surgery on the cervical spine, conservative options are often initially pursued. Observing for 4-6 weeks may be the initial step. Nonsteroidal anti-inflammatory medications or Tyenol may be tried. We try to initially avoid narcotic or muscle relaxant medications. Failure to improve may warrant physical therapy, chiropractor therapy or acupuncture. Eventually, an MRI can be performed to evaluate for nerve compression from disc bulges or herniations, bone spurs, or other compression forces. Even though it is not FDA approved, injections may be pursued.
RMBSI Board Certified surgeons routinely perform ACDFs
If a patient fails conservative options or the patient has significant weakness or numbness, surgery may be considered. Surgical options include posterior tubular minimally invasive foraminotomy, ACDF, or artificial disc replacement (ACDR). Posterior minimally invasive foraminotomy can be a reasonable option in a young person with good cervical curvature (lordosis) and a specific type of nerve compression to the side of the spinal cord in the foramen. However about 15-20% of the time patients develop increased neck pain and spasms about 6 months after the surgery. ACDR is also a good option in a younger patient with only 1 or 2 spine levels requiring surgery. Posterior cervical decompression and fusion does a poor job of improving lordosis, but can supplement ACDF or be used for failed prior fusions (pseudoarthrosis). ACDF, however, can be performed much more universally for many different conditions. It is the “workhorse” procedure for the cervical spine.
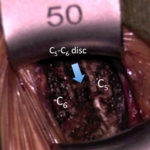
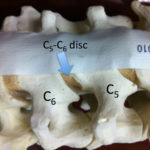
In an ACDF, an incision is made in the front of the neck. The neck organs and blood vessels are retracted to the side. The disc(s) are completely removed and a bone or prosthetic spacer is placed between the vertebral bones. A plate and screws are usually placed to hold the bones in place while the bones grow together, or fuse. While the nerve decompression and plate/ screws are placed during surgery, the fusion does not actually occur for 6-12 months.
 ACDF is one of the most common procedures performed in the cervical spine. Due to the fact that the spinal cord cannot be manipulated without causing spinal cord injury, there is a limited role for posterior decompression-alone procedures in the neck. This is much different than the lower lumbar spine in which the spinal cord has ended above this region and the nerve roots can be manipulated to perform decompressions and discectomies. Lumbar decompressions are common.
ACDF is one of the most common procedures performed in the cervical spine. Due to the fact that the spinal cord cannot be manipulated without causing spinal cord injury, there is a limited role for posterior decompression-alone procedures in the neck. This is much different than the lower lumbar spine in which the spinal cord has ended above this region and the nerve roots can be manipulated to perform decompressions and discectomies. Lumbar decompressions are common.