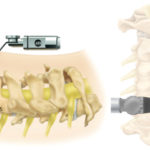
 Traditionally cervical (neck) spine surgery has been performed “open”. The two main surgical options historically have been fusion and decompression. Neither has been very minimally invasive.
Traditionally cervical (neck) spine surgery has been performed “open”. The two main surgical options historically have been fusion and decompression. Neither has been very minimally invasive.
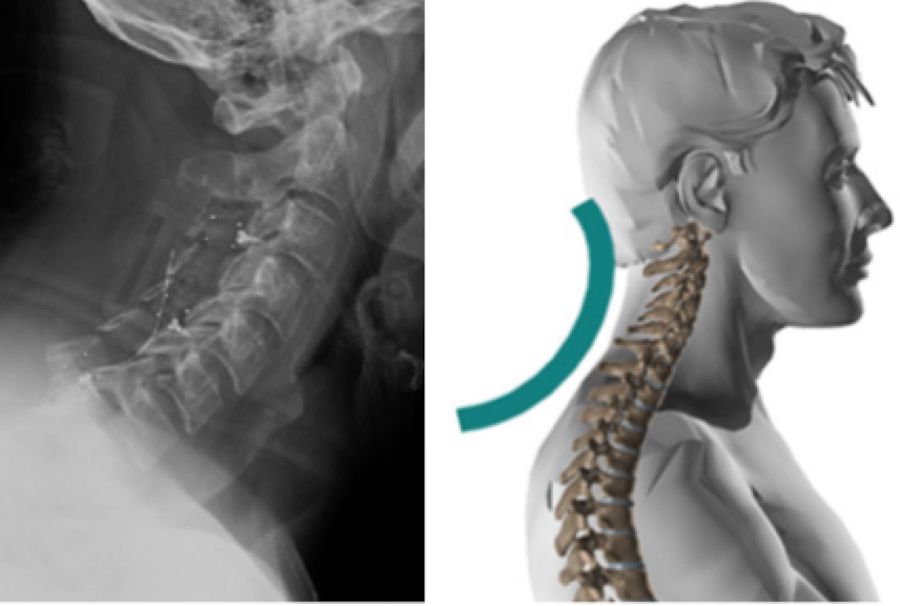
Unlike the lumbar spine (low back), multiple level cervical decompressions without fusion are not commonly performed anymore. Laminectomy (decompression) alone has been shown in many cases to lead to pain over time and other symptoms. Patients may develop “postlaminectomy kyphosis”, which is a condition in which the patient’s head starts to fall forward and the patient loses their normal neck curvature. Placing screws and rods in the back of the neck help prevents this, but again, this is not minimally invasive.