 As we get older, we all develop “changes” in our spines. Studies have shown that about 30% of completely pain-free (asymptomatic) people undergoing a lumbar MRI have abnormalities detected. After the age of 60 years old, about 90% of people have at least a “degenerative disc”.
As we get older, we all develop “changes” in our spines. Studies have shown that about 30% of completely pain-free (asymptomatic) people undergoing a lumbar MRI have abnormalities detected. After the age of 60 years old, about 90% of people have at least a “degenerative disc”.
Low back pain is one of the most common diseases in the United States. Low back and leg pain can be caused by a spine problem such as a bone spur or disc herniation, but can also be caused by hip problems, pelvic problems, kidney problems, muscle problems or unknown reasons. Regardless of the cause, the vast majority of people get better with just rest, time and over-the-counter medicines.
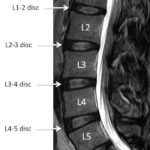
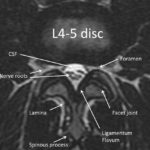
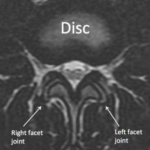
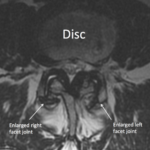
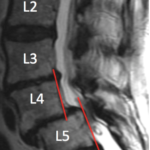
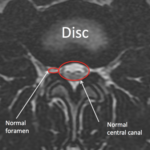
While we try to limit ordering MRIs on everyone with low back or leg pain until the symptoms are persistent for weeks to months, conservative options such as physical therapy have failed or weakness/ numbness develops, many people have MRIs. It’s pretty common nowadays for patients to receive their MRI report and most people read these reports and try to understand what is wrong. With the ease of internet access, self diagnosis is very common. What’s important to remember is that the report is made by a radiologist (a physician specifically trained to review these images) who legally must report everything observed. The radiologist makes this report often without any consideration of patient’s symptoms. Therefore the MRI report may mention many different findings or abnormalities, making patients feel like everything is wrong with their spine. However all, none or some of these findings may explain your symptoms. Additionally, the severity of findings is very subjective and may differ between physicians. It’s imperative that you discuss the MRI report with a spine specialist to see which, if any, of these findings are important and need to be addressed. The spine specialist should review the actual images with you and answer any questions you have about your report. If surgery eventually is required, surgery is intended to only fix the issues causing the symptoms and not to make your spine or MRI look perfect.