Prior to permanent implantation, a neuropsychiatric evaluation is mandated by insurance companies. This is not meant to imply that patients are “crazy” or have psychiatric problems. However many patients with pain have depression, anxiety and poor coping which can limit the effectiveness of the device. This screening both helps patients prepare for the spinal cord stimulator and identifies some patients that may not respond as well.
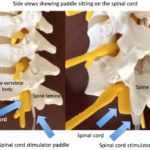
If it is decided to pursue a spinal cord stimulation, Rocky Mountain Brain & Spine Institute can place the permanent implant. This usually is a paddle (larger than the electrodes used in the trial). A laminectomy is performed and the paddle is placed over the spinal cord. The wires are then connected to a battery which usually sits in the buttock.
The permanent spinal cord stimulation procedure can be performed as an outpatient procedure, but some patients are observed over night. Some patients can even undergo the procedure awake, with some sedation.
The spinal cord stimulator battery will eventually need to be replaced ever 6-10 years. There are rechargeable versions, but even these eventually require replacement, which is a repeat outpatient surgery.
Spinal cord stimulators now can be MRI compatible.
If you have questions about spinal cord stimulation, contact our BOARD CERTIFIED spine surgeon at Rocky Mountain Brain & Spine Institute.