
In 2021, Cosmopolitan magazine posted multiple “covers”, under the cloak, “11 women who prove wellness isn’t ‘one size fits all’”.
From the Baroque period to about 1910, obesity was perceived as a sign of wealth and attractiveness. Renoir famously painted numerous “Bathers” scenes of obese individuals into the late 1800s. However it was “Rubenesque” full-figured women, by Dutch painter Sir Peter Rubens in the 1600s, which first depicted the idealization.
First of all, there is a difference between “health” and “wellness”. The World Health Organization (WHO) defines “health” as a, “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. “Wellness”, on the other hand, is a poorly defined term, but generally is an active process of growth involving a balance of various aspects of your life. Smoking is a good example to differentiate the two. Quitting smoking indisputably will improve one’s health. However if there are other ongoing spiritual, emotional, occupational, intellectual, environmental or social issues, then quitting smoking may not necessarily improve one’s wellness.

The continuous pursuit of fitness has existed since prehistoric times. Originally for hunting and gathering, fitness is now for living longer without disease and feeling better as we live. However as more Americans have found difficulty fitting the criteria, some have tried to move the “bar” regarding what our medical system deems “healthy”. For example, normal blood pressure previously used less than 120 mmHg as the high systolic (top) number and 80 mmHg as the diastolic (bottom) number. The American Society of Hypertension knew that the risk of cardiovascular disease begins around 115/75 mmHg, and doubles with each 20 mmHg increment higher. Partially due to this being difficult to achieve, 140/90 suddenly became the “new” normal in the early 2000s. It wasn’t that the Newton’s Laws of gravity no longer applied to earth… Americans became unhealthy. Patients were depressed at hearing they were hypertensive, and doctors were depressed because angry patients didn’t want to hear about their hypertension. Luckily, in 2017, the American Heart Association admitted the complications of this change and readjusted back to 130/80. In 2020, we are finally back down to 120/80 as the upper limit of “healthy” blood pressure.

A well-known comedian previously satirically summarized similar societal negotiations on health and fitness, in the context of the rope in gym class. The gym rope was “… that unclimbable symbol of aspiration and frustration…”. For decades, many elementary school and junior high school students had trouble climbing the gym rope, and some were embarrassed by failure. But instead to promoting health when summiting failed, by encouraging perseverance with strengthening and weight loss, society just removed the rope from schools altogether. Kids can’t fail climbing the gym rope if there is no gym rope… This type of response to declining societal health, especially in kids, has been harmful.
Since the 1970s, obesity in America has increased. Just like hypertension, medical providers focus less on weight, so patients may think their “muffin top” is the new norm. After all, everyone knows that the best part of a muffin is its top!!! But about 70% of Americans are either overweight or obese and this is linked to numerous diseases, including more than 14 types of cancers, with brain meningiomas and gliomas being just two. The estimated medical cost of prevention, diagnosis, and treatment is about $150 billion per year. And we know that it’s not specifically a body mass index (BMI), but fat pannus that marks obesity and drives its deleterious course. It is especially shocking in 2021 that a popular magazine would pictorialize obesity and caption, “This is healthy!” Our current COVID-19 pandemic is directly related to increased weight. Obesity increased the risk of severe illness from COVID-19, triples the risk of hospitalization, increases the risk of death, and lowers the chance of vaccine response. Therefore, more than ever, we should be promoting weight loss.
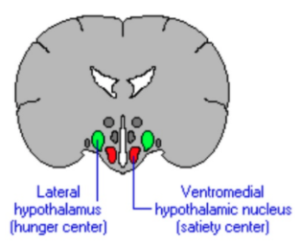
 Despite the commercialization, there is no solid evidence that any diet fads curb obesity. The it likely because some components of weight balance are in our brains. Our hypothalamus is the integrative area with a “feeding center” and “satiety center”. Our energy expenditure, in comparison to our nutrient intake, helps our brains know if we should be hungry or full.
Despite the commercialization, there is no solid evidence that any diet fads curb obesity. The it likely because some components of weight balance are in our brains. Our hypothalamus is the integrative area with a “feeding center” and “satiety center”. Our energy expenditure, in comparison to our nutrient intake, helps our brains know if we should be hungry or full.
However we also have “reward” centers in our brain, near the ventral striatum. Turns out that the inexpensive, super convenient, high-calorie food, cleverly marketed to consumers, is full of easily digestible fat and sugars, which provides more reward than less digestible Brussel sprouts loaded with vitamins and minerals. As a result, few Americans really want to overeat, especially fattening foods, but we still do because our subconscious brain undermines our intentions.
This is also why traditional weight loss surgery, which primarily shrink the stomach’s volume, seem to be ineffective. Changing the amount of food a body can intake or absorb, in no way affects the brain’s reward pathways driving obesity. Patients may temporarily eat less after gastric bypass, but they constantly struggle with wanting to eat more.
As indicated in a prior RMBSI blog, deep brain stimulation of the lateral hypothalamus, via stimulatory inhibition, has been shown to diminish food intake by blocking the brain control centers. But how many people are willing to go so far as to have stimulators inserted in their brains?
From a complication perspective, obesity is a significant risk factor in neurosurgical procedures. In spinal surgery, increased body mass index risks surgical site infection, venous blood clots, peripheral nerve compression during surgery, major medical complications, prolonged length of surgery and hospital stay, and potentially worse functional outcomes. There’s a higher risk of reoperation and revision surgery. Cranial surgery has similar risks.
Obesity may be related to neurodegenerative conditions. Fat, called adipose tissue, may not just be “fat storage”, but an actual body organ releasing hormones. Midlife obesity can lead to the development of Alzheimer disease, now considered, “type 3 diabetes”, because obese people are at such higher risk of developing the disease. “Lipid rafts” may be responsible for the amyloid plaques built up in Alzheimer brains. Although the link is less apparent, being overweight is more prevalent in patients with Parkinson’s disease.
In summary we know that obesity is surely not healthy, but what is its relationship to wellness? This is far more complicated. Obesity is not a true psychological disorder, but many clinicians argue it likely is a mental or behavioral issue. Some studies find that mental distress predicts being overweight or weight gain, while other studies find no association between weight status and psychological health. However, obese individuals are up to five times more likely to report lower global quality of life to those of healthy-weight.
This being said, there is a growing sentiment that stopping a societal focus on weight could decrease psychological discontent or body-image problems. This is likely the message Cosmopolitan magazine is promoting… Let’s stop criticizing body mass so overweight people feel better about themselves. However, ending public weight bias or thin-ideal messages is such a small fraction of one person’s overall wellness. Some overweight-obese people feel psychologically healthy in an obesogenic environment, because obesity may actually be a freely chosen personal attribute, although somewhat irrational. Their obesity may not register, for now, on their scale of self-actualization.
“Rubensian beauty” is a direct path to many neurologic and global health problems. In both spine and cranial surgery, these patients risk complications and poor outcomes. Any suggesting of improved wellness, is likely short-lived and misperceived. Wellness does not need to be one-size-fits-all, however excess body fat is a small sliver of the wellness tree that should not be callously ignored or carelessly encouraged.






