 Millennials seem to want to change everything… or do they?
Millennials seem to want to change everything… or do they?
Recently we’ve learned that about 88% of Millennials (born 1981 to 1996) prefer texting over phone calls, with about 52% feeling anxious on the phone. They just don’t seem to like direct contact with other humans. In contrast, 77% of Baby Boomers (born 1946-1964) enjoy speaking on the telephone.
About 60% of Millennials say they dread making a call to set a doctor’s appointment and about half still have their parents make the call for them. Most Baby Boomers can’t schedule enough office visits with their medical providers… almost characterizing their doctor visit as a pre-party-like social event before their “senior supper”.
Telehealth medicine has surprisingly been around for a while. An 1879 article in the Lancet talked about using the telephone to reduce unnecessary office visits (Alexander Graham Bell’s patent was in 1876). In 1925, a cover of Science and Invention magazine showed a patient being diagnosed remotely, using a device called a “teledactyl”, which would allow doctors not only see the patient through a viewscreen but touch them with robot arms in their home.
The most common use of telemedicine in the last few decades was to treat chronic diseases, mostly in rural areas of the country. The 100 million Americans with chronic disease account for about 75% of health care expenditures. Traditionally, chronic disease was managed through frequent office-based models, often for simple tasks like blood pressure measurement. Especially in remote communities, this travel was simply not feasible or cost effective. Telehealth visits with home blood pressure monitoring was a very successful alternative.
 During COVID-19, telehealth medicine drastically increased in both rural and urban settings. Many primary care clinics closed during shutdowns, and even specialists like neurosurgery clinics maintained continuity of postoperative care or routine follow-up by virtual means. The only option for offering outpatient healthcare was to utilize telemedicine.
During COVID-19, telehealth medicine drastically increased in both rural and urban settings. Many primary care clinics closed during shutdowns, and even specialists like neurosurgery clinics maintained continuity of postoperative care or routine follow-up by virtual means. The only option for offering outpatient healthcare was to utilize telemedicine.
As I began using phone and virtual visits infrequently in my clinic, I forecasted numerous problems. I assumed that patients wanted to physically be in front of a doctor, and would be displeased with the informality of a phone call. I felt my ability to evaluate a patient was best accomplished in person… I could note subtle nuances or exam findings cluing a diagnosis, not achievable amid a physical separation.
However, studies post- 2020 COVID indicate that all generations, from Boomers to Millennials, seem to want more convenient and effective communication options. Currently, 20% of Boomers, 44% of Gen Xers, and 42% of Millennials are likely to switch practices unless they get it. Sixty percent of Gen X and 70% of Millennials even want online, email and text communication options.
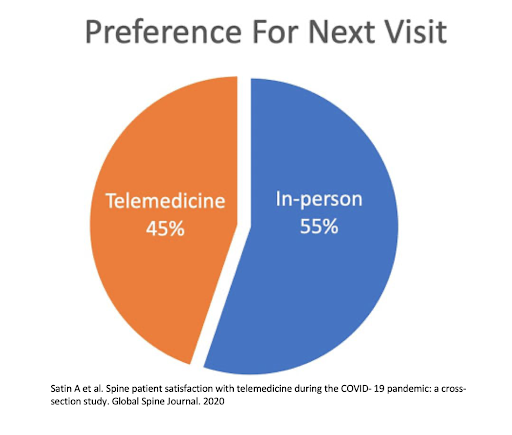 Newer 2021 studies are showing that telemedicine use in spine medicine is not only generally successful, but met with high satisfaction from patients. In one Global Spine Journal study, 70% of respondents reported a 4 out of 5 level of satisfaction, with 45% indicating a preference for virtual visits over in-person. Realistically, in postoperative spine patients, pain scores and analgesic consumption are the two most common variables in outcome research, and both are easily obtainable via telemedicine. It does not appear that neurologic examination is compromised with remote visits. Instead of testing muscle strength by palpating resistance across a joint, observing functional muscle use with the patient using household objects may arguably be a more practical exam. Sensory testing has always been subjective, so this is no different in person or by webcam. Postoperative problems do not appear to be missed, which would lead to subsequent intervention. Additional studies are showing reduced cost with this approach.
Newer 2021 studies are showing that telemedicine use in spine medicine is not only generally successful, but met with high satisfaction from patients. In one Global Spine Journal study, 70% of respondents reported a 4 out of 5 level of satisfaction, with 45% indicating a preference for virtual visits over in-person. Realistically, in postoperative spine patients, pain scores and analgesic consumption are the two most common variables in outcome research, and both are easily obtainable via telemedicine. It does not appear that neurologic examination is compromised with remote visits. Instead of testing muscle strength by palpating resistance across a joint, observing functional muscle use with the patient using household objects may arguably be a more practical exam. Sensory testing has always been subjective, so this is no different in person or by webcam. Postoperative problems do not appear to be missed, which would lead to subsequent intervention. Additional studies are showing reduced cost with this approach.
It appears that telemedicine has been around long before Millennials, and will continue past Gen Z’ers. Further studies and developed of guidelines with infrastructure will be needed to boost the utility of consistent and safe telehealth.
 According to Harvard Business Review, “In a few years, the idea of receiving medical treatment exclusively at a doctor’s office or hospital will seem quaint”. Neurosurgeons, in particular, have always been characterized as having poor bedside manner and awkward social skills. If any medical specialty should embrace virtual visits, maybe it should be neurosurgery.
According to Harvard Business Review, “In a few years, the idea of receiving medical treatment exclusively at a doctor’s office or hospital will seem quaint”. Neurosurgeons, in particular, have always been characterized as having poor bedside manner and awkward social skills. If any medical specialty should embrace virtual visits, maybe it should be neurosurgery.






