Photo credit orthoinfo.aaos.com
Conservative treatment is often tried before considering low back surgery. Time, anti-inflammatory medication, physical therapy, yoga, and injections are reasonable modalities. Even after surgery, adjuvant options may be considered.
Often when patients present in a neurosurgery clinic, they have already tried injections and ponder if they have pursued enough to consider surgery. It’s not uncommon for their pain management specialist to still be offering even more injections.
So at what point has a patient failed the injection route, and simply is being turned into swiss cheese with all the needle stick holes? It’s no longer pain management, but more like caseiculture?
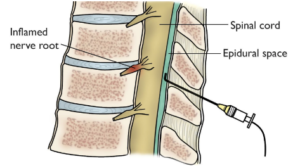
Lumbar epidural steroid injections (ESIs) often involve injecting a steroid and/or numbing medication into the epidural space, around the spinal nerves. This often is a good option to treat leg pain.
Despite numerous studies demonstrating the effectiveness of ESIs, no evidence-based guidelines address a definite dose or frequency. According to the North American Spine Society (NASS) 2013 statement, transforaminal ESI is effective in providing greater than 50% pain relief for at least one month, with half of these patients continuing to benefit from treatment for a year or more. Some even argue the pain relief should be closer to 80% for longer than 6-8 weeks. NASS also recommends no more than three injections within six months, for a recommended maximum of 6 injections per year.
If an injection fails, then repeating the injection is controversial. Not uncommonly, even a failed single injection may suggest the patient should move on to another option. On the other hand, if the injection is successful but temporary, then how many times should this option be repeated? After all, steroid injections have been shown to elevated blood glucose, affect the risk of cataract formation and affect the bone mineral density and fracture risk. Providers need to make the best efforts to limit the total steroid dose while achieving optimal outcomes.
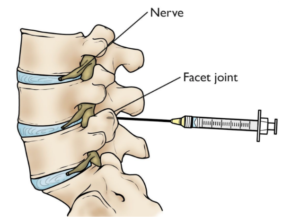
Photo credit orthoinfo.aaos.com
A recent 2020 survey amongst the Spine Intervention Society members shows quite a bit of variation. ~90% of proceduralists may be using a steroid dose higher than necessary. Yet nearly 90% are otherwise adhering to the yearly frequency recommended by NASS. Only 8% offer 7+ injections per year and 3% offer more than 10 + injections per year. Interestingly, this study showed private practice proceduralists may offer 50% more injections than academic providers (at a university). Unfortunately, this study did not address how many years a patient should pursue up to 6 injections.
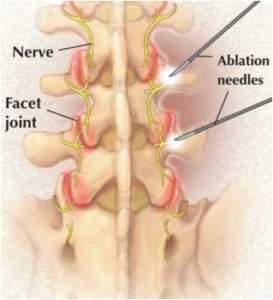
Lumbar facet injections often involve injecting a steroid and/or numbing medication into the facet joint. A medial branch block (MBB) injects just a numbing medication around the joint, often to determine the need for radiofrequency ablation (RFA). An RFA involves burning that nerve, although the nerve can “regrow”. This often is an option to treat back pain. Facet-mediated pain may be a controversial topic. The literature suggests that the lumbar facets may account for 15-45% of low back pain, however, there may be no effective correlation between symptoms and changes in imaging. Facet arthritis is a common finding and may be asymptomatic. Some proceduralists still diagnose facet symptoms, even with a normal-appearing facet.
A recent 2020 study assessed the practice of multiple facet injections, MBBs or RFAs.
 It appears that for a single facet injection, there can be a favorable outcome, but rarely for longer than 3 months. The literature on repeated facet injections is weak. Repeat facet injections can provide remarkable immediate pain relief, but with significantly less benefit when used up to, or longer than, 6 months. Therefore facet injections likely should be offered once, with the expectation that it will not be long-lasting. If multiple are offered, about 3 months should be the cutoff for when to move on to another treatment option. Unfortunately, surveys indicate 30% of patients receive 3 or more repeat facet injections in 1 year, which may not follow these practice recommendations.
It appears that for a single facet injection, there can be a favorable outcome, but rarely for longer than 3 months. The literature on repeated facet injections is weak. Repeat facet injections can provide remarkable immediate pain relief, but with significantly less benefit when used up to, or longer than, 6 months. Therefore facet injections likely should be offered once, with the expectation that it will not be long-lasting. If multiple are offered, about 3 months should be the cutoff for when to move on to another treatment option. Unfortunately, surveys indicate 30% of patients receive 3 or more repeat facet injections in 1 year, which may not follow these practice recommendations.
MBBs only use a local anesthetic. If the patient has 70-80% pain relief from the MBB, RFAs may be offered. There is little evidence to support more than 2 MBBs.
RFA may improve pain for 6-12 months, and some studies indicate relief over 3 years. There may be a greater likelihood of long-term improvement if the RFA is repeated, due to re-growth of the medial branch nerve. Additional RFA treatments may be associated with another 10-16 months of improvements, but only in patients who received a benefit from the first procedure. The nice part about RFA is that it may not require a steroid. However, there is no definitive recommendation in the literature for the total number of RFA procedures before a patient should consider other options. RFAs likely should not be repeated for years on end.
Of course, RFA has not been shown to be effective for discogenic low back pain.
References:
- Vydra D et al. Current trends in steroid dose choice and frequency of administration of epidural steroid injections: a survey study. PNR 12, 2020
- Onafowokan O et al. Multiple injections for low back pain: what’s the future? European Spine Journal. 2020.






