Lumbar fusion is a common procedure.
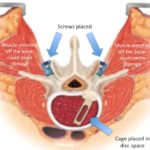
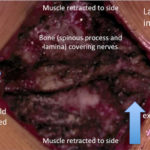
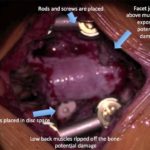
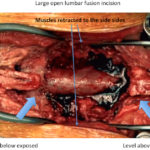
In many cases, lumbar decompression can improve leg and some back symptoms. However in certain circumstances, fusion is required. The most common reason for fusion is abnormal slippage of one vertebral bone over another (spondylolisthesis).
In a recent study, Ghogawala et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. NEJM, 374(15):1424-1434, 2016, it was demonstrated that pain was significantly better with fusion as compared to decompression alone.
The initial treatment is still often conservative. Observation with or without over-the-counter anti-inflammatories or Tylenol may be tried. Sometimes patients try chiropractors or acupuncture. With persistent symptoms, therapy may be the next option. If after a few weeks symptoms are still intractable, then advanced imaging like a spine x-ray or spine MRI may be pursued. If the MRI shows an abnormal slippage and nerve compression, injections may be tried. Usually conservative options are tried before considering surgery. In certain circumstances, imaging and surgery are sought sooner.